The best start in life comes from a good education, a safe, stable home and being part of a community that supports our children and young people.
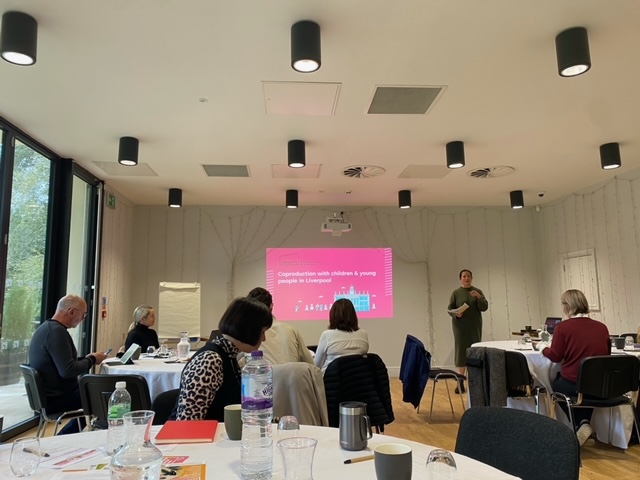
That’s the vision of Liverpool’s Children and Young People’s Partnership (LCYP), a partnership made up of Liverpool City Council, Alder Hey, Merseycare, the University of Liverpool, Merseyside Police, local primary and secondary schools and third sector organisations.
Continue reading